Introduction
Epstein Barr Virus (EBV) related T and NK malignancies, such as extra-nodal NK/T lymphoma (ENKTL) or chronic active EBV (CAEBV), are intrinsically chemoresistant. Conventionally, this is overcome in the clinic by using high-intensity treatment protocols. However, this makes therapy difficult to deliver, especially in patients with co-morbidities, and there are few options for those with relapsed or refractory disease. Intrinsic resistance to apoptosis, driven primarily by the anti-apoptotic BH3 protein BCL-XL, appears to play a significant part in treatment resistance (Sejic, Blood Advances 2020). However, inhibition of anti-apoptotic pathways alone cannot kill all malignant cells in vitro and is not curative in animal models. Identification of drugs that function synergistically with BCL-XL inhibition is critical to unlocking the chemoresistance. We investigated the combination of BH3 inhibition with the promotion of apoptosis using the antibody-drug conjugate (ADC) Brentuximab Vedotin (BV). BV delivers an MMAE payload to CD30-positive cells triggering apoptotic cell death through cell cycle arrest and DNA damage. We identified synergism between BV and a BCL-XL BH3 mimetic that dramatically increased cell death at concentrations that should limit on-target toxicity.
Methods
A diverse panel of EBV+ T/NK lymphoma cell lines including SNK1, MECO4, SNK6, SNT8, SNK10, SNT15 and SNT16 were evaluated for sensitivity to MMAE alone and with specific BH3 family inhibitors including A1331852, inhibiting BCL-XL, venetoclax inhibiting and BCL-2 and the MCL-1 inhibitor S63845 (Generon). Drug sensitivity was assessed by staining with PI/Annexin (eBioscience) and then analysing on an Accuri C6 flow cytometer. Cell surface expression of CD30 was assessed by flow cytometry (eBiosience). We then tested the effect of BV in combination with A1331852 and assessed for the effect on viability using CellTitre Glo (Promega).
Results
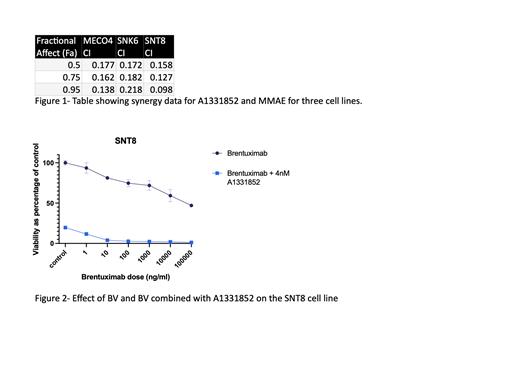
Single-agent MMAE was toxic to all cell lines tested with an LD50 ranging from 0.6-33 nM and a maximal killing effect between 10%-45%.PI/Annexin staining suggested the mode of cell killing was apoptotic. As a single agent, A1331852 showed efficacy across all cell lines, apart from MEC04 which exhibited reduced susceptibility. In combination with MMAE, A1331852 enhanced both the sensitivity and maximal killing effect seen. Using a 1:50 fixed dose ratio then analysis in CompuSyn the effect of both agents was synergistic with a fraction affect (0.5) between 0.158 and 0.177 in the cell lines tested (Figure1) . Single-agent inhibition of BCL-2 or MCL-1 showed only limited efficacy and no synergy with MMAE. High levels of CD30 expression was evident on all cell lines making ENKTL a viable target for BV. While BV showed efficacy as a single agent, cell viability at a clinically achievable 100 ug/ml dose was between 30% and 78% after 72h. However, in combination with A1331852 at a low 4 nM dose maximal viability was between 1% and 25%, figure 2 shows results for the SNT8 cell line. In most resistant lines, SNK6 and MECO4, sensitivity to BV could be increased using doses of A1331852 up to 500 nM, leading to 5-6% viability at 72h. Based on murine PK data this should still be clinically achievable.
Discussion
Combining targeted delivery of MMAE via BV with the BCL-XL inhibitor A1331852 is highly toxic to a panel of CAEBV and ENKTL-derived cell lines. These cells are intrinsically resistant to apoptosis but are sensitive to BCL-XL inhibition. The use of BCL-XL inhibitors has been limited by on-target thrombocytopenia and the combination of BH3 mimetics with chemotherapy can cause marked haematological toxicity. Therefore, using a targeted agent such BV in combination with BCL-XL inhibition has the potential to enhance efficacy without triggering excessive toxicity. Additionally, the synergistic nature of the combination allows the use of low-dose A1331852. We are working to better understand the cell line-specific differences in resistance to combination therapy, which does not appear to relate to either baseline BCL-XL protein levels, CD30 expression or the rate of cell division.
These data show the potential of BV with BCL-XL inhibition to be an effective and tolerable treatment for ENKTL. We are now planning a detailed preclinical study to better understand the efficacy and safety of this combination in vivo and progress towards a future clinical trial.
OffLabel Disclosure:
Glover:Jansen: Research Funding. Fox:AbbVie: Consultancy; Genmab: Consultancy, Membership on an entity's Board of Directors or advisory committees. Shannon-Lowe:Jansen: Research Funding.
Brentuximab Vedotin in EBV related T and NK neoplasms

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal